Managing Chronic Kidney Disease: Essential Lifestyle Changes and Effective Treatment Options

Chronic kidney disease (CKD) is a long-term condition characterized by the gradual loss of kidney function over time. It affects millions of people worldwide and can lead to serious health complications if not managed effectively. Early detection and lifestyle modifications can significantly impact the progression of the disease and improve the quality of life for those affected. This article discusses essential lifestyle changes and treatment options for managing chronic kidney disease.
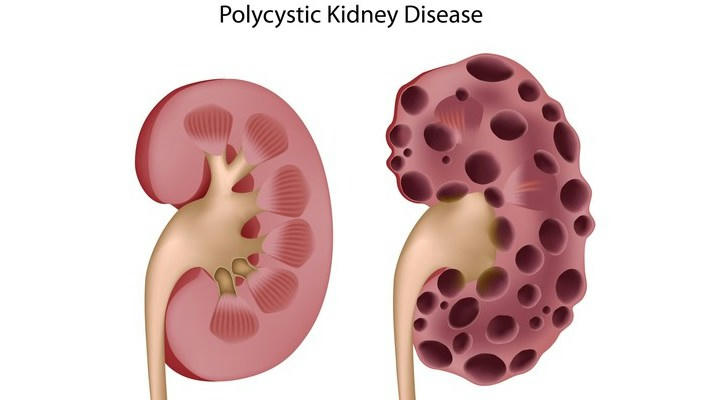
Understanding Chronic Kidney Disease
Before diving into management strategies, it’s important to understand what CKD is. The kidneys play a crucial role in filtering waste and excess fluid from the blood, balancing electrolytes, and regulating blood pressure. When kidney function declines, waste products can build up in the body, leading to various health issues. CKD is often categorized into five stages, with stage five indicating end-stage renal disease (ESRD), where dialysis or kidney transplantation may be necessary.
Lifestyle Changes to Manage CKD
1. Dietary Modifications
One of the most significant changes individuals with CKD can make is adjusting their diet. A renal diet typically involves the following components:
Limiting Sodium Intake: Reducing sodium helps manage blood pressure and decreases fluid retention. Patients are advised to avoid processed foods, canned soups, and salty snacks.
Controlling Protein Consumption: While protein is essential for health, excessive intake can strain the kidneys. It’s important to choose high-quality protein sources, such as lean meats and fish, and consume them in moderation.
Monitoring Potassium and Phosphorus Levels: High levels of potassium and phosphorus can be harmful to those with CKD. Foods rich in potassium (like bananas and potatoes) and phosphorus (like dairy products and certain grains) may need to be limited.
Staying Hydrated: Adequate fluid intake is essential, but some patients may need to limit their fluid intake depending on their kidney function and stage of CKD.
2. Regular Exercise
Physical activity is beneficial for overall health and can help manage CKD. Regular exercise can improve cardiovascular health, control weight, and enhance mood. Patients are encouraged to engage in at least 150 minutes of moderate-intensity aerobic activity each week. Activities like walking, swimming, and cycling are excellent options. It’s essential for individuals to consult their healthcare provider before starting any new exercise regimen.
3. Managing Comorbid Conditions
CKD often coexists with other health conditions such as diabetes and hypertension. Managing these comorbidities is critical to slowing the progression of kidney disease. For instance:
Diabetes Management: Keeping blood sugar levels within the target range can help protect kidney function. Regular monitoring, a balanced diet, and adherence to prescribed medications are vital.
Blood Pressure Control: High blood pressure can worsen kidney damage. Patients are often prescribed antihypertensive medications and advised to adopt lifestyle changes to maintain blood pressure within a healthy range.

4. Avoiding Harmful Substances
Certain substances can exacerbate kidney damage. Patients should avoid:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Common pain relievers like ibuprofen and naproxen can harm the kidneys, especially when taken regularly.
Excessive Alcohol: While moderate alcohol consumption may be acceptable for some, excessive drinking can contribute to kidney damage and other health problems.
Tobacco: Smoking is harmful to overall health and can worsen kidney function. Quitting smoking is one of the best things individuals can do for their health.
Treatment Options for CKD
1. Medications
Several medications can help manage CKD and its complications:
ACE Inhibitors and ARBs: These medications help control blood pressure and protect kidney function, especially in diabetic patients.
Diuretics: These can help reduce fluid retention and manage blood pressure.
Phosphate Binders: For patients with elevated phosphorus levels, these medications help control phosphate levels in the blood.
Erythropoiesis-Stimulating Agents: For those with anemia due to CKD, these medications stimulate the production of red blood cells.
2. Regular Monitoring
Regular check-ups and lab tests are essential for managing CKD. Patients should work closely with their healthcare team to monitor kidney function, blood pressure, and electrolyte levels. Adjustments to treatment plans can be made based on these evaluations.
3. Dialysis and Kidney Transplantation
In advanced stages of CKD (stage four and five), dialysis or kidney transplantation may become necessary.
Dialysis: This procedure helps filter waste and excess fluid from the blood when the kidneys can no longer perform this function. There are two types: hemodialysis and peritoneal dialysis.
Kidney Transplantation: A kidney transplant involves receiving a healthy kidney from a donor. This option can significantly improve quality of life for those with end-stage renal disease.
Managing chronic kidney disease requires a comprehensive approach that includes lifestyle changes and medical treatment. By adopting a kidney-friendly diet, engaging in regular physical activity, managing coexisting health conditions, and avoiding harmful substances, individuals can significantly improve their health outcomes. Additionally, regular monitoring and appropriate medical interventions are vital in slowing the progression of CKD. Ultimately, a proactive and informed approach can lead to better management of chronic kidney disease and an improved quality of life for those affected.
